FEATURED PRESS

PTI with Guest Frank Osborne, Founder of HawkGrips and Action Medical Technologies
Vickie Dills of Physical Therapy Innovations sits down with Frank Osborne, the Founder & CEO of HawkGrips, for an insightful podcast interview. Osborne delves into HawkGrips' evolution into a prominent figure in IASTM and beyond since its start in 2010. From serving prestigious healthcare institutions to providing diverse education resources, HawkGrips continues to innovate and support professionals in the field of physical therapy and beyond.
Physical Therapy Innovations

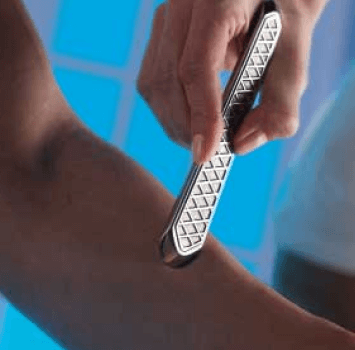
Instrument Assisted Soft Tissue Mobilization
This edition of The Newsletter of The American Society of Hand Therapists gives a comprehensive exploration of Instrument-Assisted Soft Tissue Mobilization (IASTM), authored by Jyo Supnekar, OTR/L, CHT, CLT, Clinical Specialist from Johns Hopkins Hospital. The article has a focus on HawkGrips as a prominent brand in the IASTM landscape.
ASHT Times

Playing Injured
Major League Lacrosse athlete Paul Rabil reflects on his experience playing through injuries while simultaneously prioritizing his health. He highlights the role of HawkGrips IASTM in his routine, alongside Johns Hopkins Hospital physical therapy specialist Ken Johnson.
The Players Tribune


Getting a Grip
This article details the remarkable story of Frank “Oz” Osborne ‘96, a Saint Joseph’s University alum, whose pursuit of pain relief evolved into the creation of HawkGrips.
Saint Joseph’s University

Garage Gym Reviews
Cooper Mitchell from Garage Gym Reviews shares his personal experience with IASTM and asserts that HawkGrips “are the best IASTM tools money can buy.” He gives a comprehensive review, where he provides an in-depth analysis of the tools collectively and evaluates each individual instrument’s unique features and effectiveness.
Garage Gym Reviews
HawkGrips: Beyond Perfection
Rehab Insider highlights the journey of HawkGrips, chronicling how Frank Osborne’s struggle with pain inspired the creation of these innovative stainless steel instruments. Endorsed in this feature by therapists at Phoenix Rehabilitation and Health Services, HawkGrips have become synonymous with superior patient care.
Rehab Insider

Deep Impact: Instrument-assisted soft tissue mobilization zeroes in on restrictions to promote healing
This piece provides a comprehensive exploration of IASTM and highlights its positive influence on functional outcomes and patient well-being. The authors, based on their clinical experiences, endorse IASTM as a vital therapeutic enhancement, with HawkGrips recognized as unmatched soft tissue instruments globally.
ADVANCE for Physical Therapy & Rehab Medicine


Providing the tools to help others heal
Frank Osborne, the founder of HawkGrips, shares his remarkable journey from a devastating skiing accident to creating stainless-steel tools for soft-tissue rehabilitation. Learn how HawkGrips challenges industry standards, embodying resilience and innovation in the field.
The Philadelphia Inquirer
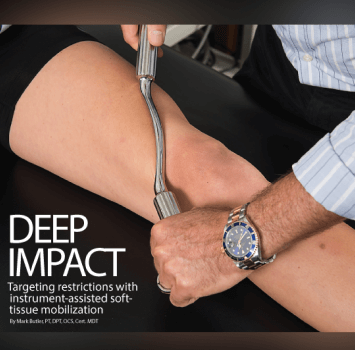
Deep Impact: Targeting restrictions with instrument-assisted soft-tissue mobilization
This feature delves into the growing popularity of Instrument-Assisted Soft-Tissue Mobilization (IASTM) in the realm of manual therapy. It explores IASTM’s history, current evidence base, impact on patient healing, and showcases HawkGrips photos throughout.
ADVANCE for Physical Therapy & Rehab Medicine Philadelphia Inquirer
HawkGrips: Getting a Grip on Soft Tissue Injuries
Steve Smith, Physical Therapist with the Los Angeles Dodgers, shares his HawkGrips journey. Since discovering these instruments, he has never looked back.
Steve Smith, PT, DPT, SCS, CSCS NEXT LINE → Major League Physical Therapist for the Los Angeles Dodgers
